About GARDASIL 9
GARDASIL® 9 (Human Papillomavirus 9 valent Vaccine) (Recombinant, adsorbed)
Prescribing Information (Great Britain) & Prescribing Information (Northern Ireland) [External links]
GARDASIL® 9 is indicated for active immunisation of individuals from the age of 9 years, against the following HPV diseases:1
- GARDASIL 9 Summary of Product Characteristics.
- Hartwig S et al. Estimation of the epidemiological burden of HPV-related anogenital cancers, precancerous lesions, and genital warts in women and men in Europe: potential additional benefit of a nine-valent second generation HPV vaccine compared to first generation HPV vaccines. Papillomavirus Res 2015; 1:90–100.
a) With data from: Cervical cancer: Sanjose S et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study.
Lancet Oncol. 2010;11(11):1048–1056. Anal cancer: Alemany L et al. Human papillomavirus DNA prevalence and type distribution in anal carcinomas worldwide. Int J Cancer. 2015;136(1):98–107.
Vaginal cancer: Alemany L et al. Large contribution of human papillomavirus in vaginal neoplastic lesions: a worldwide study in 597 samples. Eur J Cancer. 2014;50(16):2846–2854.
Vulvar cancer: de Sanjose S et al. Worldwide human p papillomavirus genotype attribution in over 2000 cases of intraepithelial and invasive lesions of the vulva. Eur J Cancer. 2013;49(16):3450–3461
b) Method for the calculation for precancerous lesions: Based on the data from five countries (France, Denmark, Iceland, Norway, and Sweden) incidence rate ranges were estimated for CIN2+ by age groups, which were then extrapolated to the combined female population of the 32 included countries. The estimates for VIN2/3 and VaIN2/3 were extrapolated from data from Nygard study (2014) from Denmark, Iceland, and Norway from the period 2004 2006. For the estimation of AIN2/3, sex-specific, age-standardised incidence rates from the Danish Registry of Pathology were used, extrapolated to the female and the male population, respectively, of all 32 European countries.
What HPV types does GARDASIL® 9 help protect against?1,2
GARDASIL® 9 combines
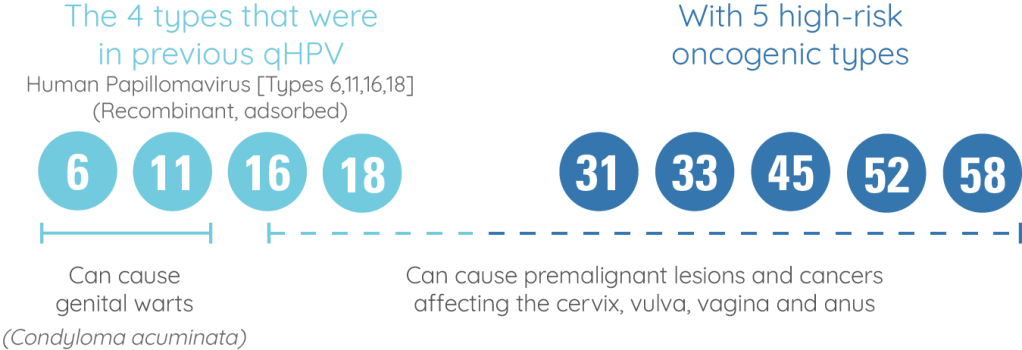
GARDASIL® 9 provides

*Phase 3 randomised, double-blind, efficacy, immunogenicity, and safety study. Participants (women aged 16 – 26 [N=14,204]) received three intramuscular injections of the GARDASIL® 9 vaccine (9vHPV) or GARDASIL® (qHPV) at Day 1, Month 2, and Month 6. Efficacy was assessed after a follow-up of up to 67 months after Dose 3 (median follow-up 43 months after Dose 3). The primary outcomes were efficacy of 9vHPV vaccine versus qHPV vaccine to prevent the combined endpoint of high-grade cervical disease (cervical intraepithelial neoplasia Grade 2 or 3, adenocarcinoma in situ, invasive cervical carcinoma), vulvar disease (vulvar intraepithelial neoplasia Grade 2/3, vulvar cancer), and vaginal disease (vaginal intraepithelial neoplasia Grade 2/3, vaginal cancer) related to HPV 31, 33, 45, 52, and 58 and non-inferiority (excluding a decrease of 1·5 times) of HPV 6, 11, 16, and 18 antibody geometric mean titres (GMTs) compared with qHPV vaccine. The PPE population consisted of individuals who received all 3 vaccinations within one year of enrolment, did not have major deviations from the study protocol were naïve (PCR negative and seronegative) to the relevant HPV type(s) (31, 33, 45, 52 and 58) prior to dose one and remained PCR negative to the relevant HPV type(s) through one month post Dose 3 (month 7).
Event rate = 1/6016 in the GARDASIL® 9 group (n=7099) vs. 38/6017 in the GARDASIL® group (n=7105)
‘Worse’ is defined as:
HPV 31-, 33-, 45-, 52-, 58-related CIN 2/3, AIS, cervical cancer, VIN 2/3, VaIN 2/3, vulvar cancer, and vaginal cancer.†
† No cases of cervical cancer, VIN2/3, vulvar and vaginal cancer were diagnosed in the PPE (Per Protocol Efficacy) population.
Please refer to the Summary of Product Characteristics for full prescribing information.
Please refer to the Summary of Product Characteristics for full prescribing information.
Hypersensitivity to the active substances or to any of the excipients. Individuals with hypersensitivity after previous administration of GARDASIL® 9 or GARDASIL®/Silgard* should not receive GARDASIL® 9 *Silgard (Human papillomavirus vaccine [types 6, 11, 16, 18] (recombinant, absorbed)) (Silgard is not licensed in the UK).
Please refer to the Summary of Product Characteristics for full prescribing information.
Safety and immunogenicity in individuals who have received immunoglobulin or blood-derived products during the 3 months prior to vaccination have not been studied in clinical trials.
Use with other vaccines
GARDASIL® 9 may be administered concomitantly with a combined booster vaccine containing diphtheria (d) and tetanus (T) with either pertussis [acellular, component] (ap) and/or poliomyelitis [inactivated] (IPV) (dTap, dT-IPV, dTap-IPV vaccines) with no significant interference with antibody response to any of the components of either vaccine. This is based on the results from a clinical trial in which a combined dTap-IPV vaccine was administered concomitantly with the first dose of GARDASIL® 9.
Use with hormonal contraceptives
In clinical studies, 60.2% of women aged 16 through 26 years who received GARDASIL® 9 used hormonal contraceptives during the vaccination period of the clinical studies. Use of hormonal contraceptives did not appear to affect the type specific immune responses to GARDASIL® 9.
Please refer to the Summary of Product Characteristics for full prescribing information.
| Side effects of HPV vaccination | |
|---|---|
| Very common side effects (occurring in ≥ 10% of people) | ● Pain, redness and swelling at the injection site ● Headache |
| Common side effects (occurring in ≥ 1% to < 10% of people) | ● Bruising, or itching at the injection site ● Dizziness ● Nausea ● Fever ● Fatigue |
A full list of side effects can be found in the Summary of Product Characteristics and Patient Information Leaflet.
Useful links
Change to the vaccine: the vaccine supplied for the National Immunisation Programme will change from GARDASIL® to GARDASIL® 9 during the 2021 to 2022 academic year. Public Health England (PHE) will continue to supply vaccine for the HPV programme in the usual way.
For more information please click here.
References
Supporting documentation
GARDASIL® 9 (Human Papillomavirus 9 valent Vaccine) (Recombinant, adsorbed)
Prescribing Information (Great Britain) & Prescribing Information (Northern Ireland) [External links]
By clicking the links above you will leave the MSD Connect website and be taken to the emc PI portal website
