Primary Care HPV Vaccination Resources
Primary Care HPV Vaccination Resources
Confidently support HPV vaccination with knowledge and tools for primary care professionals
These resources provide practical guidance to address common questions, manage vaccine hesitancy and deliver clear, evidence-based information to patients and their families – helping you to focus on providing the best care.
HPV Vaccination:
What do I need to know?
This resource provides primary care professionals with essential knowledge about HPV, the proven benefits of vaccination and the public health impact of HPV immunisation in reducing certain cancer rates and improving patient outcomes.

What is Human Papillomavirus (HPV)?

Human papillomavirus (HPV) is a double-stranded DNA virus that infects the skin and mucosae of the upper respiratory and anogenital tracts1

HPV viruses are classified as either ‘high-risk’ or ‘low-risk’ types, depending on their association with the development of HPV-related cancers1
There are around 100 types of HPV, of which ~40 infect the genital tract1

HPV is associated with certain cancers, including of the cervix, vulva, vagina, and anus1,2
Who can be affected by HPV?

HPV poses risks to both men and women1

4 out of 5 sexually active individuals may become infected with at least one type of HPV at some point in their lives3
For most people, HPV clears on its own.
But for those who don’t clear the virus, it can cause certain cancers and diseases.1
What are the risks of HPV?

A minority of persistent infections with high-risk HPV types will eventually lead to certain HPV-related cancers, however, these infections may lay dormant for 20 years or more2
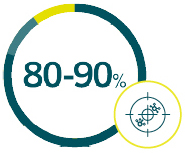
of all anal cancers are associated with HPV infection, with HPV16 and HPV18 accounting for the majority of anal cancers1

Low-risk HPV types can lead to
genital warts, which is the most
commonly diagnosed viral sexually
transmitted infection in the UK2
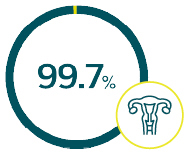
of cervical cancer cases are caused by persistent infection with high-risk HPV types4

HPV16 and HPV18 account for almost 80% of all invasive cervical cancers in the UK5
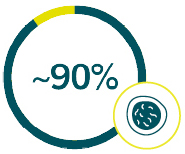
of all genital warts are caused by HPV6 and HPV111
More than 80 million people have been vaccinated against HPV worldwide since 20086

Over 10 million doses of HPV vaccines have been given in the UK in over 10 years6

Cervical cancer rates have been reduced by almost 90% in women in their 20s who were offered the HPV vaccination at age 12 and 13 years in England, when compared with an unvaccinated population7*
Between 2011 and 2014, the national uptake of HPV vaccination in England for girls aged 12–13 years was consistently >85%, with over 40% of Primary Care Trusts in England achieving at least 90%8
*An observational study in England estimated the relative risk of cervical cancer in vaccinated cohorts compared with earlier cohorts who were not eligible for HPV vaccination. Data from a population-based cancer registry were extracted on Jan 26, 2021, and were assessed for diagnoses of cervical cancer and CIN3 from Jan 1, 2006 to June 30, 2019 in women aged 20-64 years. 13.7 million-years of follow up data were used. The study estimated that cervical cancer rates have been reduced by 87% in women aged 20 years to younger than 30 years who were offered HPV vaccination between 12 and 13 years of age, compared with an unvaccinated population7
HPV vaccination: Why is there still an unmet need?

HPV vaccine uptake in the UK declined since the start of the SARS-CoV-2 pandemic in early 2020 due to school closures9

In England during 2024, over 25% of girls and over 30% of boys aged 13–14 years in year 9 have not received their HPV vaccine9
HPV vaccine first dose uptake rates in Year 8 pupils aged 12–13 years in England:9
2020–2021
76.6% of girls
71.0% of boys9
2021–2022
69.6% of girls
62.4% of boys99
2022–2023
71.3% of girls
65.2% of boys9
2023–2024
72.9% of girls
67.7% of boys9

Vaccination can protect against certain HPV related cancers and diseases
Through your efforts in ensuring eligible young people receive HPV vaccination, YOU are:

Protecting boys and girls from certain HPV-related cancers and genital warts in the community and nationally1,10

Reducing the burden on NHS resource and costs, by preventing certain HPV-related cancers11,12

Helping save the lives of around 850 women per year13

School and primary care nurses have an important role in educating young people about HPV and offering HPV vaccination to eligible people15,16
Early protection with HPV vaccination in young boys and girls can prevent them from getting certain HPV-related cancers later in life10,13
Without prevention and screening, women may face more intensive diagnostics, treatment, emotional stress, and health risks16

- UK Health Security Agency. Human Papillomavirus (HPV): the green book, chapter 18a. June 2023. Available at: https://www.gov.uk/government/publications/human-papillomavirus-hpv-the-green-book-chapter-18a. Last accessed: October 2025.
-
National Cancer Institute. HPV and Cancer. April 2023. Available at: https://www.cancer.gov/about-cancer/causes-prevention/
risk/infectious-agents/hpv-and-cancer. Last accessed: October 2025. - Cheeson HW, et al. Sex Transm Dis. 2014;4(11):660–4.
- Okunade KS. J Obstet Gynaecol. 2020;40:602–8. 5. The Catalan Institute of Oncology and the International Agency for Research on Cancer Information Centre on HPV and Cancer. United Kingdom Human Papillomavirus and Related Cancers, Fact Sheet 2023. March 2023. Available at: https://hpvcentre.net/statistics/reports/GBR_FS.pdf. Last accessed: October 2025.
- The Catalan Institute of Oncology and the International Agency for Re-search on Cancer Information Centre on HPV and Cancer. United Kingdom Human Papillomavirus and Related Cancers, Fact Sheet 2023. March 2023. Available at: https://hpvcentre.net/statistics/reports/GBR_FS.pdf. Last accessed: November 2025.
- UK Health Security Agency. Information on HPV vaccination: Available at: https://www.gov.uk/government/publications/hpv-vaccine-vaccination-guide-leaflet/information-on-the-hpv-vaccination-from-september-2023. Last accessed: October 2025
- Falcaro M, et al. Lancet. 2021; 389:2084–2092.
- Public Health England. Human papillomavirus (HPV) immunisation programme review: 2008 to 2014. March 2015. Available at: https://www.gov.uk/government/publications/human-papillomavirus-hpv-immunisation-programme-review-2008-to-2014. Last accessed: October 2025.
-
UKHSA Human papillomavirus (HPV) vaccination coverage in adolescents in England: 2023 to 2024. Human papillomavirus (HPV) vaccination coverage in adolescents in England: 2023 to 2024 – Available at:
https://assets.publishing.service.gov.uk/media/5c4f232ced915d7d3953d207/HPV_Vaccine_Coverage_in_England_200809_to_201314.pdf. Last accessed: October 2025. - UK Health Security Agency. Press Release: Concern over drop in HPV vaccine coverage among secondary school pupils. January 2023. Available at: https://www.gov.uk/government/news/concern-over-drop-in-hpv-vaccine-coverage-among-secondary-school-pupils. Last accessed: October 2025.
- Jit et al. BMJ. 2008; 337:a769.
- Fabiano et al. Eur J Health Econ. 2023; 24:75–80.
-
UK Health Security Agency. Ten years on since the start of the HPV vaccine programme – what impact is it having? July 2018. Available at:
https://ukhsa.blog.gov.uk/2018/06/18/ten-years-on-since-the-start-of-the-hpv-vaccine-programme-what-impact-is-it-having/. Last accessed: October 2025. - Hilton et al. BMC Infectious Diseases. 2011; 11:226.
- Boyce et al. PLOS ONE. 2012; 7(9):e43416.
- NHS England and Department of Health and Social Care (2025). Cervical screening care pathway. GOV.UK. Available at: https://www.gov.uk/government/publications/cervical-screening-care-pathway/cervical-screening-care-pathway. Accessed November 2025.
From missed to protected: How Primary Care can close the HPV gap
Practical strategies for primary care teams to identify eligible individuals, optimise delivery systems and collaborate with school immunisation services to improve HPV vaccination uptake among young people aged 12–25.

How can you help protect people against certain HPV-related cancers?

Both school immunisation teams and primary care teams have an important role in offering HPV vaccination to potentially eligible people1,2

The HPV programme is primarily delivered by School Age Immunisation Services (SAIS), however provision can vary from area to area3,4

Some young people miss their immunisation in school and may not be proactively offered HPV vaccination after leaving full-time education
That’s where primary care comes in

Provide young people with a second chance to receive their HPV vaccination

School nurses have a role in making young people aware that they should contact their GP if they have missed their vaccination in school

GP practices can offer HPV vaccination opportunistically or on request to potentially eligible people aged between 14 and 25 years who missed their scheduled vaccination in school2

Vaccines given to eligible young people in General Practice will attract an item of service fee of £10.06 per dose administered2,5
Prepare your practice to deliver HPV vaccination to eligible young people who have missed their vaccination in school
01
Set HPV immunisation goals in your practice
Examples could include:

Ensuring all potentially eligible people registered in the GP practice have been vaccinated against HPV

Maximising practice remuneration by ensuring systems are in place to claim payment for HPV vaccination activity2,5
02
Ensure HPV immunisation delivery arrangements are in place

Identify a named lead member of staff with responsibility for the immunisation service and ensure all practice staff know who this lead person is2

Ensure a registered healthcare professional trained and competent in immunisation is available all or most of the time the GP practice is open2

Ensure timely appointments that are convenient to the eligible practice population2
03
Identify people who are potentially eligible to receive HPV vaccination

Create a system for identifying those potentially eligible for HPV vaccination who may attend the practice for other reasons, such as an appointment with the GP or physiotherapist. An example could be using IT alerts to remind staff to discuss HPV vaccination with potentially eligible people

If HPV immunisation is not recorded on an eligible patient’s GP record, check the HPV immunisation status with the local Child Health Information System or Child Health department2
04
Ensure all GP staff are aware of their responsibilities when it comes to HPV vaccination
Responsibilities could include:

Checking in advance HPV immunisation history
of young people attending the practice for other vaccinations, such as annual influenza vaccination, or healthcare provisions, such as cervical cancer screening, contraceptive reviews and medication reviews

Ensuring local healthcare providers who may engage with young people, such as pharmacists, physiotherapists and opticians, are aware that your GP practice offers HPV vaccination to eligible young people aged between 14
and 25 years who have missed their HPV vaccination in school

Ensuring practice business meetings include
HPV vaccination on the agenda

Ensure people aged 12–13 years are referred to the School Age
Immunisation Services

Ensure groups eligible for vaccination via sexual health services are informed of this arrangement
- UK Health Security Agency. Human Papillomavirus (HPV): the green book, chapter 18a. June 2023. Available at: https://www.gov.uk/government/publications/human-papillomavirus-hpv-the-green-book-chapter-18a. Last accessed: October 2025.
- NHS England and NHS Improvement. GP letter on vaccination and immunisation changes for 2021/22. March 2021. Available at: https://www.england.nhs.uk/wp-content/uploads/2021/03/B0434_Update-on-vaccination-and-immunisation-changes-for-202122-v4.pdf. Last accessed: October 2025.
-
UK Health Security Agency. Human papillomavirus (HPV) vaccine coverage estimates
in England: 2020 to 2021. December 2021. Available at: https://www.gov.uk/government/statistics/human-papillomavirus-hpv-vaccine-
coverage-estimates. Last accessed: October 2025. - UK Health Security Agency. Supporting Immunisation Programmes. February 2023. Available at: https://www.gov.uk/government/publications/health-protection-in-schools-and-other-childcarefacilities/supporting-immunisation-programmes. Last accessed: October 2025.
- NHS England. Changes to the GP Contract in 2023/24. Available at: https://www.england.nhs.uk/long-read/changes-to-the-gp-contract-in-2023-24/#immunisations-and-vaccinations. Last accessed: October 2025.
- GARDASIL9 Summary of Product Characteristics.
Discussion Guide
This PDF contains practical strategies for primary care teams to identify eligible individuals, optimise delivery systems and collaborate with school immunisation services to improve HPV vaccination uptake among young people aged 12–25.

Don’t miss out on supporting the eligible population this HPV vaccination season
As an HPV immuniser, get answers for the population’s concerns – right at your fingertips.
Join your fellow immunisation colleagues already using practical checklists, discussion guides, and FAQs to confidently address HPV vaccine hesitancy.
✅ Based on public‑health guidance (UKHSA, NHS, ECDC, WHO)
✅ Tailored for HPV immunisers
✅ Sign up in one minute!
You can unsubscribe at any time. Privacy Policy
Falling through the cracks
Every year thousands of young women aged 18–24 miss HPV vaccination. See how Nurses like you can help to identify and reach eligible patients aged 14 to under 25 before they fall through the cracks.
Supporting documentation
GARDASIL® 9 (Human Papillomavirus 9 valent Vaccine) (Recombinant, adsorbed)
Prescribing Information [External link]
By clicking the link above you will leave the MSD Connect website and be taken to the emc PI portal website
