SOME THINGS
ARE JUST PART
OF GROWING UP
WITH VARIVAX,
CHICKENPOX DOESN’T
ALWAYS HAVE TO BE
ONE OF THEM.
Prescribing Information [External link]
WITH VARIVAX,
CHICKENPOX DOESN’T
ALWAYS HAVE TO BE
ONE OF THEM.
You can also order supplies by calling the Alliance Healthcare Customer Services Team on 0330 100 0448. Please note you will need an Alliance account to order.
Data presented below/hereafter focus on immunocompetent populations aged 12 months to 12 years.
VARIVAX is indicated for vaccination against chickenpox in individuals from 12 months of age. VARIVAX can be administered to infants from 9 months of age under special circumstances, such as to conform with national vaccination schedules or in outbreak situations.1
Two doses of VARIVAX should be given to ensure optimal protection against chickenpox:1
VARIVAX is indicated for vaccination against chickenpox in individuals from 12 months of age. VARIVAX can be administered to infants from 9 months of age under special circumstances, such as to conform with national vaccination schedules or in outbreak situations.1
Two doses of VARIVAX should be given to ensure optimal protection against chickenpox:1
The most common adverse events reported in the 42 days after each injection were soreness, erythema, swelling, rash, upper respiratory illness, cough, fatigue, irritability/nervousness, disturbed sleep and diarrhoea.3
Please refer to the Summary of Product Characteristics for full details on the safety profile.
Please refer to the Summary of Product Characteristics for full prescribing information.
Please refer to the Summary of Product Characteristics for full prescribing information.
VARIVAX must not be mixed with any other vaccine or other medicinal product in the same syringe. Other injectable vaccines or other medicinal products must be given as separate injections and at different
body sites.
Concomitant administration with other vaccines
VARIVAX has been administered to toddlers at the same time as, but at a different injection site from, a combined measles, mumps, and rubella vaccine, Haemophilus influenzae type b conjugate vaccine, hepatitis B vaccine, diphtheria/tetanus/whole-cell pertussis vaccine, and oral polio virus vaccine. There was no evidence of a clinically relevant difference in the immune responses to any of the antigens when co-administered with VARIVAX. If varicella vaccine (live) strain found in VARIVAX is not given concomitantly with measles, mumps, and rubella virus vaccine live, a 1-month interval between the 2 live virus vaccines should be observed. Concurrent administration of VARIVAX and tetravalent, pentavalent or hexavalent (diphtheria, tetanus, and acellular pertussis [DTaP])-based vaccines has not been evaluated. Vaccination should be deferred for at least 5 months following blood or plasma transfusions, or administration of normal human immune globulin or varicella zoster immune globulin (VZIG). Administration of varicella zoster virus antibody-containing blood products, including VZIG or other immune globulin preparations, within 1 month following a dose of VARIVAX may reduce the immune response to the vaccine and hence reduce its protective efficacy. Therefore, administration of any of these products should be avoided within 1 month after a dose of VARIVAX unless considered to be essential. Vaccine recipients should avoid use of salicylates for 6 weeks after vaccination with VARIVAX as Reye syndrome has been reported following use of salicylates during wild-type varicella infection.
Please refer to the Summary of Product Characteristics for full prescribing information.
Side effects of VARIVAX
Healthy individuals 12 months to 12 years of age (2 doses received ≥ 3 months apart)
The following serious adverse events temporally associated with the vaccination were reported in individuals 12 months to 12 years of age given varicella vaccine (live): diarrhoea, febrile seizure, fever, post-infectious arthritis, vomiting.
The rates of systemic clinical adverse events after a second dose of VARIVAX were generally similar to, or lower than, those seen with the first dose. The rates of injection-site reactions (primarily erythema and swelling) were higher after a second dose.
A full list of side effects can be found in the Summary of Product Characteristics and Patient Information Leaflet.
Ngai AL, et al.3
A multicentre study comparing the safety and immunogenicity profiles of one- and two-dose regimens of VARIVAX in healthy children aged 12 months to 12 years. The study aimed to determine whether two doses administered 3 months apart yielded improved seroconversion rates, antibody titres or cellular immune responses to varicella. 2196 children were randomised to receive one (n=1103) or two (n=1093) doses of VARIVAX. All participants were followed for clinical reactions for 42 days after each injection and participants were asked to report any cases of varicella or zoster at any time post-vaccination. Blood samples were obtained from all children within 2 weeks before the first injection and at approximately 6 weeks after each injection to determine immunogenicity of the vaccine. In a subset of the centres, blood samples were obtained from children who seroconverted 1 year after the first injection to ascertain persistence of antibody.
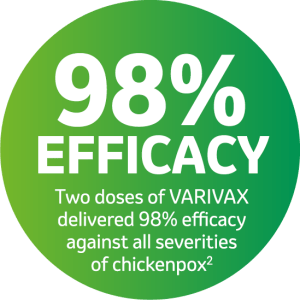
Kuter B, et al.2
A multicentre study to conduct a 9- to 10-year follow-up of a cohort of children who were randomised in 1991 to 1993 to receive either one (n=1114) or two (n=1102) doses of VARIVAX 3 months apart. The rate of varicella >42 days post-vaccination, vaccine efficacy and the persistence of varicella antibody were compared to assess whether a two-dose regimen yielded any significant clinical advantage. Overall vaccine efficacy was estimated as 1 – (observed average annual varicella incidence rate/age-adjusted expected annual varicella incidence rate).
NOTE: Individuals should receive two doses of VARIVAX to ensure optimal protection against varicella
Prescribing Information
By clicking the link above you will leave the MSD Connect website and be taken to the emc PI portal website
Loading...

This section of MSD Connect is an online portal containing promotional information about MSD pharmaceutical products, therapy area materials and professional resources and is intended for UK Healthcare Professionals.
To contact us please telephone 0208 154 8000 or email medicalinformationuk@msd.com | Privacy Policy | Terms of Use
GB-NON-07197 | Date of Preparation: August 2023
Merck Sharp & Dohme (UK) Limited Registered Office: 120 Moorgate, London, EC2M 6UR, United Kingdom.
Registered in England No. 233687 Copyright © 2023 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Adverse events should be reported. Reporting forms and information can be found at https://yellowcard.mhra.gov.uk or search for MHRA Yellow Card in the Google Play or Apple App Store. Adverse events should also be reported to Merck Sharp & Dohme (UK) Limited (Tel: 0208 154 8000)
This section of the website contains promotional information intended for UK Healthcare Professionals only. If you are not a UK healthcare professional, please click here. GB‑NON‑07725 | Date of Preparation: August 2023